As of September 22, 2021, The Ohio State University Wexner Medical Center has documented nearly 127 active patient transport ventilators, setting an all-time-high for in-use hospital ventilators.
As sourced from the Cleveland Clinic, a mechanical ventilator is a medical equipment machine that helps a patient breathe (ventilate) when he or she cannot breathe on his or her own for any reason. The patient is connected to the ventilator with a hollow tube (artificial airway) that can be inserted through the mouth and into their airway or directly through to the trachea by performing a tracheostomy, a surgically created artificial opening of the neck to the trachea. The ventilator will push a mixture of air and oxygen into the patient’s lungs to achieve a healthy and necessary amount of oxygen into the body. In addition, a ventilator will aid in holding constant low pressure called PEEP (positive end-expiratory pressure) to prevent the patient’s air sacs, located in the lung, from collapsing (Mechanical Ventilation). The patient will remain on the ventilator for the duration of their recovery until they improve to a state in which they can breathe on their own, without the support of the ventilator.
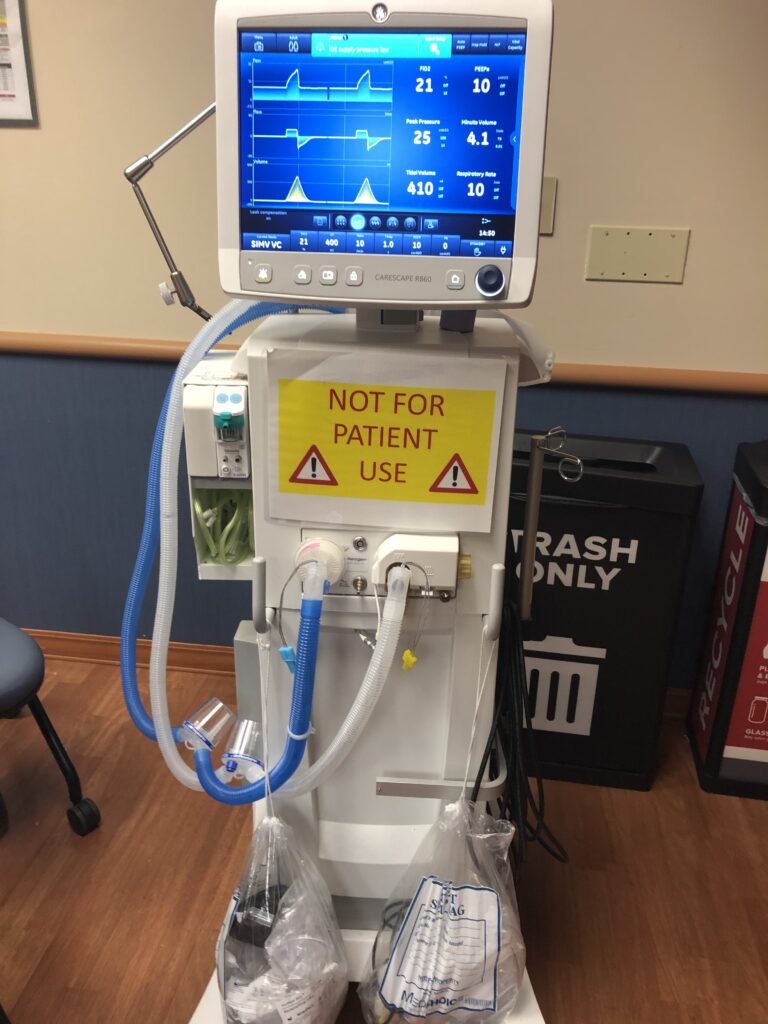
Most commonly, patients will be monitored in the Intensive Care Unit (ICU) while connected to a stationary (mechanical) ventilator with a monitor that will measure heart rate, respiratory rate, blood pressure, and oxygen saturation. The monitored levels will provide information and data to be utilized when assessing the patient and when making adjustments to the ventilator, as necessary. The destinations that will routinely occur with a patient include transportation from the ICU to imaging, CT Scan, and MRI. Such transportation processes will require the patient to be connected to a stationary ventilator, disconnected, and then re-connected to a transport ventilator. Therefore, for all patients connected to a transport ventilator, there will be continuous risks and potential complications, minor or major, that will arise and need to be addressed such as infections, collapsed lungs (pneumothorax), lung damage, medication side effects, or the inability to continue the support of the ventilator (Mechanical Ventilation).
Similar to a stationary ventilator, a transport ventilator provides ventilatory support to patients who require assistance for adequate ventilation because of illness, trauma, congenital defects, or the effects of drugs, for example anesthetics (Ventilators, transport). However, transport ventilators do, in fact, differ not only in size but in functionality and overall implementation in relation to its associated patient. In comparison, transport ventilators (Figure 2) are much smaller than stationary ventilators (Figure 1) so that such equipment devices can be placed either on the outside of the hospital bed, loosely attached, or next to the patient on top of the bed.
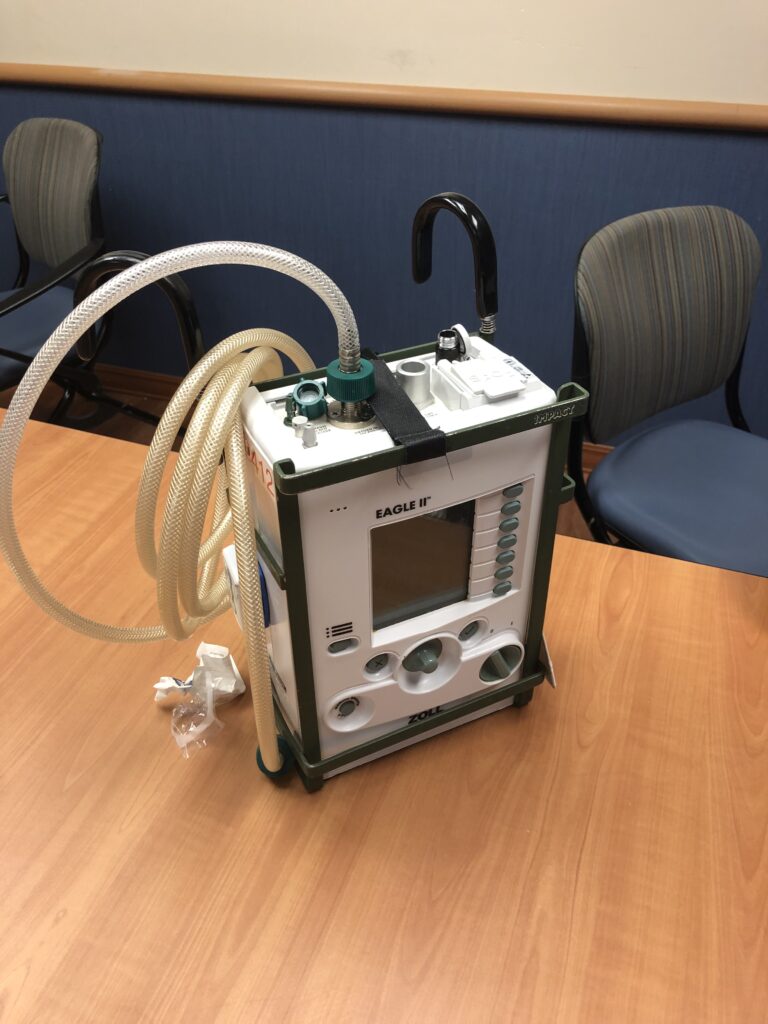
Due to the smaller size and lesser weight, the ventilator can be easily implemented in transportation throughout the hospital, removing the need to configure a solution to transport a ‘stationary’ ventilator. Additionally, a transport ventilator is intentionally designed and manufactured to take bumps and knocks as a result of the chaos that may occur during a transportation. Transport ventilators, often, will fall on the floor, be kicked, stepped on, etc., so it is crucial that the machine can take enough “accidental “damage and continue to operate with little to no handling effects. Next, the functions that are displayed in transport ventilators resemble a less complex stationary ventilator consisting of the necessary informational data enabling the nurse practitioners, respiratory therapists, and physicians to reference, interpret, and adjust accordingly to the patient.
Moreover, if an incident does take place and results in a mechanical failure, the following procedure would be to disconnect the patient and utilize an ambu bag (Figure 3) that requires the attention and operation by a bed-side nurse practitioner or respiratory therapist.

With the current process of connecting, disconnecting, and reconnecting there remains an opportunity to design a solution that will achieve a more efficient and user-friendly experience handling and implementing a transport ventilator, accounting for not only the comfort and success of the patient, but the stakeholders in the design problem consisting of the medial team of nurse practitioners, respiratory therapists, and physicians.
In collaboration with The Ohio State University Wexner Medical Center and the Osu Biomedical Engineering Team, we are seeking to redesign the user-experience of a transport ventilator in a hospital setting. Areas of focus within the scope of the problematic situation include the transport ventilators’ docking location, user-interface interaction, and tube/cord management.
Firstly, the issue in which current transport ventilators are located during transportation highlight that there truly is no designated space for the equipment machine. As previously mentioned, a transport ventilator is either (A) attached loosely onto the guide rails of the hospital bed (Figure 4) or (B) placed directly on top of the hospital bed hugging the body of the patient (Figure 5). Both placements advocate for patient discomfort and the inability to efficiently read and interact the interface of the ventilator. When transporting a patient, hospitals will display various floor elevation changes, floor terrains, hallway/doorway openings, elevator doors and depth, etc. If the ventilators are located on the perimeter of the hospital bed the possibility for the device to be hit, jostled, or knocked off increases resulting in potential mechanical failures and resorting to the use of an ambu bag, which is an option that nurse practitioners and respiratory therapists hope to avoid using on any account.


Secondly, if there is no option or hospital bed features to place a transport ventilator on the perimeter, nurses will simply place it on any available surface area of the bed that is not taken or in use by the patient. This approach, as well, continues the bumping and knocking over of the ventilator, though in this scenario the results impact the patient by receiving the hits of the ventilator contributing to even further discomfort. When limiting the line-of-sight of the nurse practitioners and respiratory therapists, who are continuously monitoring the patient during transport, the attentiveness is then taken away from the patient resulting in “unexpected events”. Overall, the current system of transporting the portable ventilator advocates for the medical team to think and act in a process that should place all the focus and attention directly on the patient and the destination intended for the patient (CT Scan, MRI, etc.).
Transitioning, the ventilator user-interface that displays patient information poses issues for the nurse practitioners who monitor the ventilator. This particular system has continuously evolved in hopes of replicating the functions and data collected as a stationary ventilator, when in the ICU. The pain points that surround this problem encompass the want of nurse practitioners to interpret the interface with their intuition, little to no questioning or thinking involved, when assessing the patient (refer back to Figure 1 & Figure 2). Even though technology will continue to advance, the need for such advancements (i.e LCD/LED screen) are not necessary when implemented in the screen of a transport ventilator, “We do not care about the guts of the machine”. The information that is necessary to be displayed should be present and made clearly known, supplemented with alarms and alerts.
To further emphasis, along with the desire to interact with a transport ventilator through efficient means, nurse practitioners have mentioned on numerous accounts, the troubles that come when receiving training from respiratory therapists to operate the advanced versions of transport ventilators. This information follows-suit with the notion that more/advancement in regard to user-interface is not always better. With more data to examine, buttons to press, and modes to adjust, the time spent on the ventilator is time wasted with monitoring the patient. This overall system, presents challenges that if addressed can create more time directed to the patient as well as stress and anxiety when fulfilling an inter-hospital transport.
The remaining focus of the problematic situation is the cord, wire, and tube management of transport ventilators (Figure 6). Currently, whether through invasive or non-invasive means, a patient when connected to a ventilator will have a breathing tube through the mouth and/or directly into the trachea. The remaining length of the tubes rest upon the patient or off to the side which presents a multitude of opportunities for the tubes and additional connective wires to be yanked, tugged, or ripped from the patient resulting in, as mentioned, manual ventilation with an ambu bag. Such complications are not only seen when in transport, but also in the Operating Room (OR) when the tubes and cords continue to lay on the patient throughout the surgical procedure.
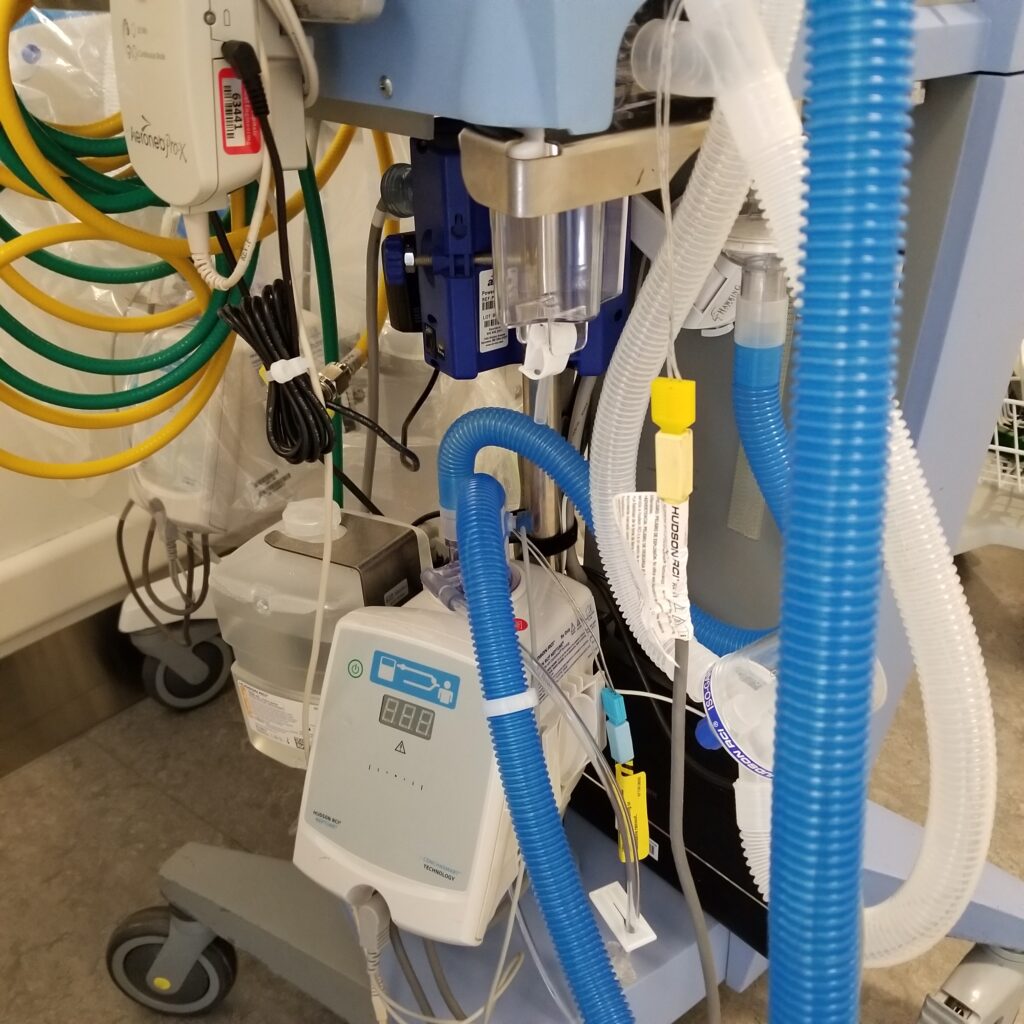
To address the cord management of transport ventilators would account for frustration, time wasted, and money saved. With limited color differences, it can be difficult amidst the chaos of transporting to distinguish certain cords and their purpose – frustration and time expended. Secondly, as previously mentioned, there are various cords and tubes which can in fact be caught onto the hospital bed or even be stepped on by the amount of foot traffic during transport. The opportunity of this issue explores the ways in which cords can be further integrated in a hospital bed to reduce frustration, time spent, and even money to replace.
To continue solution exploration, concepts developed will emphasise on the listed issues that are derived from the focus groups within the problematic situation of ventilators in a hospital setting. Overall, the goal of the redesign with the aid of the collaborative teams of the Osu Biomedical Engineering and medical staff of The Wexner Medical Center will account for the patient, primarily, as well as the supporting medical stakeholders that ensure each performed inter-hospital transport are successful. Transport ventilator docking stations, user-interfaces, and cord management all play an active role in the user-experience of ventilators, and each solution will advocate for the benefit of the intended patient and associated healthcare personnel.
Sources:
https://my.clevelandclinic.org/health/articles/15368-mechanical-ventilation
https://www.thoracic.org/patients/patient-resources/resources/mechanical-ventilation.pdf
https://www.who.int/medical_devices/innovation/hospt_equip_37.pdf?ua=1
https://image.jimcdn.com/app/cms/image/transf/dimension=origxorig:format=jpg/path/sd0158ba
42880fb5f/image/i994562bbbfc6fa87/version/1445846094/image.jpg




