Here is a hypothetical situation: you are at work one afternoon, having completed half of your workday, and your supervisor comes up to you to discuss a new task they need done by the end of the shift. The task in question is something you have not been trained for and have had no prior experience with; to complicate matters, your supervisor informs you that they do not have the tools or equipment necessary to complete it. How can you be expected to complete a task without the necessary knowledge and equipment? For many healthcare patients, this problem is extremely prevalent, especially those experiencing symptoms of arthritis. As arthritis continues to impact millions, limited access to essential medical and personal interventions prevents many from receiving the care they need, reinforcing the demand for more affordable and personalized solutions.
Arthritis is one of the most common chronic conditions, affecting over 58 million Americans, causing pain, stiffness, and reduced mobility. Managing it often requires a mix of medications, therapy, and adaptive tools, but access to these resources varies from patient to patient. For example, patients in rural areas or those with limited income often struggle to find affordable care, while expensive medications remain out of reach for many. Additionally, arthritis affects everyone differently, yet healthcare tends to rely on generalized treatments rather than personalized plans tailored to individual needs. This lack of access and personalization leaves many patients without proper support, worsening their symptoms and quality of life. Addressing these issues is essential to improving arthritis care and treatment.
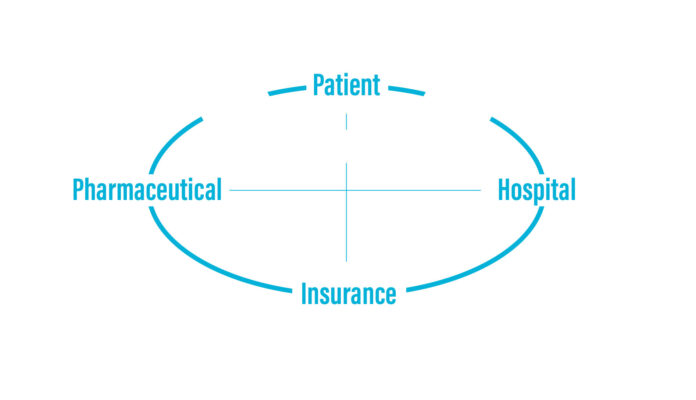
With regard to arthritis care, several key stakeholders are involved, each with unique roles and relationships. Patients are at the center, facing significant challenges due to restricted access to necessary treatments and medications. Their families are also important stakeholders, as they experience the impact of the patient’s pain and struggles, which can inhibit their own lives as they assist with daily tasks and challenges. Healthcare providers, including doctors and therapists, aim to deliver effective treatment; however, they often face constraints due to restrictions and the high cost of medications, which can limit the care options available to patients. Insurance companies prioritize saving money over personalized care, causing gaps between patients and providers, while drug companies create expensive medications that make access harder for many. The most salient issue at stake is the disparity in care resulting from financial barriers and a one-size-fits-all mentality, which prevents effective management of a condition that affects individuals in very different ways.
To understand the healthcare system, particularly in patient treatment and care, I began conducting secondary research, which included disability perspectives related to patients, healthcare industry trends from pharmaceutical and insurance viewpoints, emerging technologies, and arthritis-related pathology and treatment options.
With respect to framing the perspectives around disability and pathology, I looked into artists with different diseases, not just arthritis, and how their life was impacted by their disease; these stories pushed past the narrative of living with a disability, rather it discussed how these artists weren’t limited by their disease, but embraced it and used it to create beautiful works. In a publication, a University of Massachusetts representative details this use of disease, saying, “Most importantly, the artist highlights that a person’s disability can’t be separated from their identity and daily interactions. Disability becomes place: a place to which people migrate, and a place in which [Neil] Marcus found himself staying after he was diagnosed with a neurological disorder.” (University of Massachusetts Amherst, 2020). This quote details Neil Marcus’ journey with dystonia, and paints a portrait of both the individuality and community with regard to disease. The artistic perspective of disease and care can be pushed further than just identifying and coping with an illness; as pointed out in the VeritusArthritis blog, “From painting to writing, gardening to music, being creative can give us a much-needed distraction, relief, or even a moment of joy when we’re in pain.” (Veritus Arthritis, 2024). As living with any sort of chronic pain or illness is difficult, it falls to the patient to seek out and experience any form of joy or creative outlet necessary.
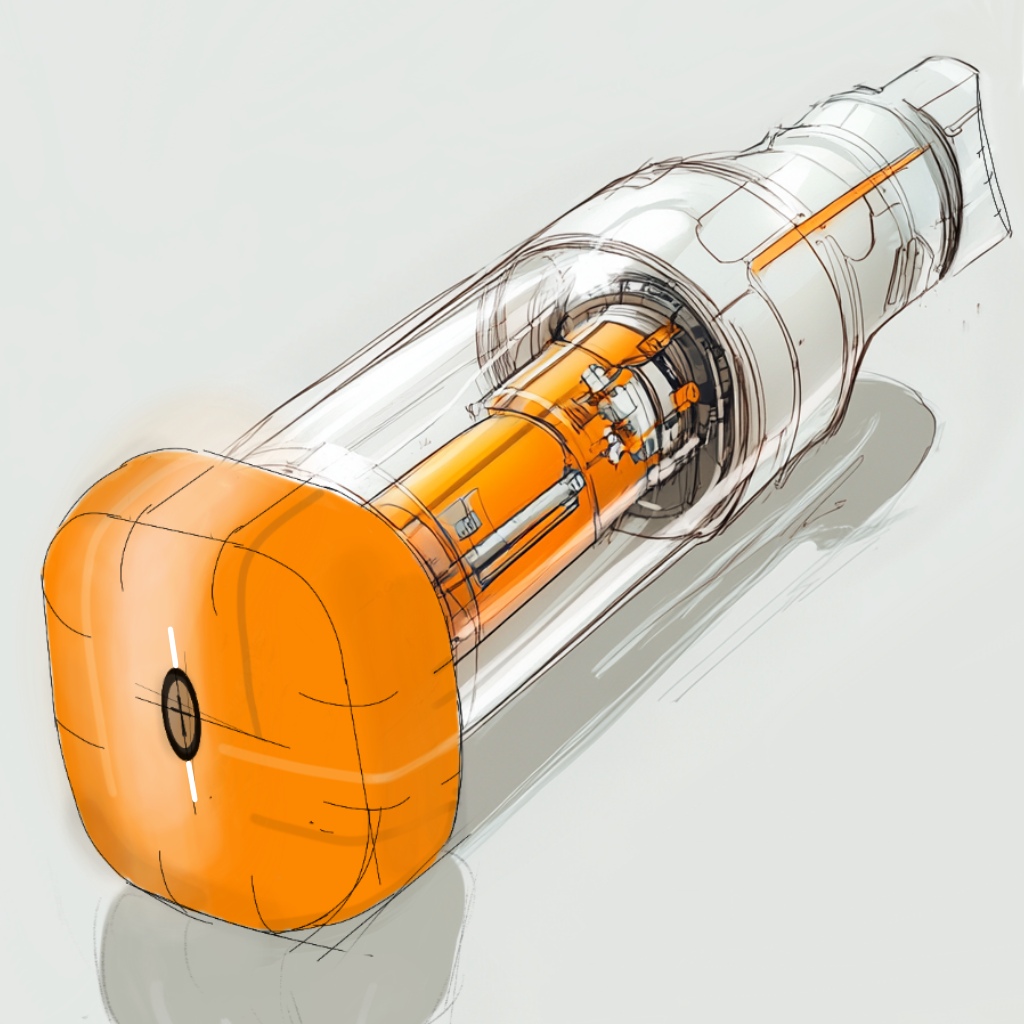
This secondary research surrounding disease perspectives helped inform one of my design conjectures. The Fast-Implement Recovery Stim Tool (FIRST) is designed for individuals who need quick relief from physical strain, whether from exercise, overwork, or injury. By allowing users to inject medication that aids in muscle and body recovery, FIRST allows people to bounce back quickly and continue their activities without extensive downtime. This autonomy is crucial for maintaining an active lifestyle, reflecting the resilience shown by artists like Van Gogh, Kusama, and Kahlo, who persevered despite their struggles. With this idea, several challenges need to be addressed for this device to be effective. Key questions include how to ensure ease of use while delivering the correct dosage of medication; considerations around different body types, metabolic rates, and potential allergies must be factored in; the device may need to incorporate various medications to meet individual needs, which highlights the scope involved in creating a versatile recovery tool.
When discussing the business aspect of disease and care, I looked into various topics, ranging from how the healthcare system is responding to the aging population to telehealth and treatment, from healthcare costs for chronic illnesses to healthcare company partnerships. These topics have provided me with a number of insights with regard to how hospitals, insurance companies, and pharmaceutical companies can better aid and assist their clients. The first insight drawn from this secondary research is that the current overall healthcare system cannot keep up with the growing number of patients and demand, especially elderly patients, who require more visits and regular check-ins. The World Health Organization published an article in which it provides statistics and discusses the aging population and healthcare, saying, “By 2030, 1 in 6 people in the world will be aged 60 years or over. At this time the share of the population aged 60 years and over will increase from 1 billion in 2020 to 1.4 billion.” (World Health Organization, 2022). It goes further, saying “Older age is also characterized by the emergence of several complex health states commonly called geriatric syndromes. They are often the consequence of multiple underlying factors and include frailty, urinary incontinence, falls, delirium and pressure ulcers.” (World Health Organization, 2022). This wide range of symptoms and limitations proves to be difficult when treating the elderly, in that the cases and symptoms range person-to person and are different on a case-by-case basis.

These insights regarding how we handle care from an administrator’s perspectives were key in my next design conjecture. The AI Healthcare Assistant is a wearable device designed to attach to clothing or be worn as a necklace. It monitors vital signs like heart rate, blood pressure, and blood flow while connecting users to local healthcare services during emergencies. While it doesn’t diagnose conditions, it shares essential patient data and facilitates communication between patients and providers. This product addresses the need for individualized care, especially for aging populations, emphasizing the importance of regular check-ins and recognizing that symptoms vary from person to person. There are challenges that arise when discussing this idea, which include ensuring the privacy and security of sensitive medical information, requiring strong data protection protocols. There’s also the risk of over-reliance on the device, which should enhance, not replace, professional medical diagnostics. The AI assistant must be seen as a supportive tool that promotes collaboration between patients and healthcare providers.
The last secondary research I would like to discuss is that of arthritis, which entails pathology, injection treatment possibilities, surgical intervention, and environmental design. As this section pertains to the focus of this project, I wanted to conduct the most research on this aspect. One of the main points discussed in the article by the John’s Hopkins Arthritis Center is that RA is driven by the immune system continuing to attack the body, even after the initial trigger may no longer be present. “Once initiated and even after a putative trigger may be eliminated, there are feed forward pathways that result in an auto-perpetuating process” (Ra Pathophysiology, 2024). This means that RA continues damaging joints and tissues due to these pathways. This adaptive and compounding threat is one that should not be taken lightly; when RA reaches a point of hindered mobility or lingering pain, some healthcare professionals will recommend surgery or more serious methods of treatment. As detailed in Smith’s paper, implantable drug delivery systems are proving to be a more beneficial form of treatment than surgeries in a lot of cases. Smith and colleagues mention, “IDDS patients had a 55% reduction in toxicity compared to 20% in the CMM group (P = 0.0003)” (Smith et al., 2005). They continue, discussing how the tests were verified, saying, “toxicities are one of the most important reasons for non-compliance with pain medicine regimens” (Smith et al., 2005). This research is crucial to the next design conjecture, while also remaining a key area of focus moving forward.

The design conjecture relating to the specific area of arthritis care and treatment is one that takes into account the pathology and environmental design aspects in the hopes of improving the quality of life of the patient. ArthAid is a supportive device designed for people with arthritis. It fits over the painful area and features an internal mechanism that provides adjustable support while using the affected limb. A dial on the device allows users to control the level of support needed for different activities, enhancing their ability to manage pain and maintain independence. This design connects to the focus of my research by integrating insights on arthritis, its causes, and treatment options, ultimately aiming to improve users’ everyday lives and overall quality of life. There are critical questions to consider in regard to ArthAid. Since ArthAid does not deliver medication, what are the long-term impacts on users? Could reliance on the sleeve lead to muscle weakness or decreased usage of the affected limb? Additionally, what are the psychological effects of using a support device? It is vital to ensure that ArthAid encourages proper movement of the affected area without fostering dependence, supporting long-term health as arthritis symptoms progress over time.
In order to better understand the daily experience of living with arthritis, I created a survey. I distributed the survey by sending a link via email to friends, family, and peers. I also reached out to arthritis foundations across North America, hoping they would share it with their networks; however, none were able to assist. Instead, I was advised to publish the survey on online forums and discussion sites like Reddit and Facebook, which turned out to be quite effective. In total, I received 91 responses, categorized into two groups: individuals with arthritis and those with close relations to someone with the condition. The survey included a range of questions covering demographics, treatment methods, and overall treatment and care satisfaction. At the end, I invited participants to connect with me via Zoom or email for follow-up interviews, and eight expressed interest in doing so. The most significant takeaway from the survey, aside from securing participants for interviews, is the comprehensive list of symptoms and treatment options that patients reported using or being prescribed. This data will guide my next phase of primary research, focusing specifically on injectable drug delivery systems.
In a world where medical advancements have made arthritis more manageable, it is unacceptable that many patients still face barriers to accessing proper care. Whether it’s a lack of affordable treatments, inadequate personal interventions, or the absence of personalized care plans, the healthcare system often falls short in addressing the unique needs of arthritis patients. By prioritizing accessibility and individualized approaches, we can bridge the gap in arthritis care, ensuring that every patient receives the support they need to live a healthier, more comfortable life. The healthcare system needs to evolve and adapt to the needs of patients, striving to promote equity among them.
References:
Distraction, expression, or a moment of joy: How creativity helps people with arthritis. Versus Arthritis. (2024, April 12). https://versusarthritis.org/news/2024/april/distraction-expression-or-a-moment-of-joy-how-creativity-helps-people-with-arthritis/
Ra Pathophysiology • Johns Hopkins Arthritis Center. Johns Hopkins Arthritis Center. (2024). https://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-pathophysiology-2/
Smith, T. J., Coyne, P. J., Staats, P. S., Deer, T., Stearns, L. J., Rauck, R. L., Boortz-Marx, R. L., Buchser, E., Català, E., Bryce, D. A., Cousins, M., & Pool, G. E. (2005). An implantable drug delivery system (idds) for refractory cancer pain provides sustained pain control, less drug-related toxicity, and possibly better survival compared with Comprehensive Medical Management (CMM). Annals of Oncology, 16(5), 825–833. https://doi.org/10.1093/annonc/mdi156
University of Massachusetts Amherst. (2020, March 19). Body/Freedom/Art: Rethinking Disability Through Art. past@present. https://umasshistory.wordpress.com/2015/08/19/bodyfreedomart-rethinking-disability-through-art/
OpenAI. (2024). ChatGPT (Sept 22 version) [Large language model]. https://chat.openai.com/chat