If you have cared for a young child while they’re sick, you know how difficult it is. They’re fussy, feverish, and fidgety, not to mention if you are cleaning up vomit and diarrhea every few hours. You’re worried about medicine intake and keeping that fever down, but you’re also home from work so you’re entertaining them while simultaneously taking conference calls on your laptop. You’re told they need electrolytes and water but they’re telling you their throat hurts too bad so you give them popsicles and their favorite juice. You don’t know if that helps, but it quiets the cries for 5 minutes. You supply a fridge full of treats and mac and cheese, anything that they will get and keep down, no matter the nutrient content. There’s no sleep, and as soon as they start to recover a few days later, the younger one coughs.


There are a few rules most parents know help cool the fevers and soothe the aches. Sick days are full of wet wash clothes, medicine regimens, temperature checks, cool bathes, and as instructed by all doctors, fluids, fluids, fluids. Hydration is one of the most important factors of everyday and lifelong health. It affects one’s body and brain from motor function and bowel movements to mental health and energy levels. When the body is already under the stress of a viral or chronic illness, hydration is at the forefront of treatment to sustain the body.
Dehydration is a loss of body fluids, which are made up of water and salts. It can cause headaches and low energy, long-term impacts such as chronic constipation, and in extreme circumstances hospitalization and kidney damage. When sick children vomit or have diarrhea, they can lose large amounts of salts and water from their bodies, and can become dehydrated very quickly.
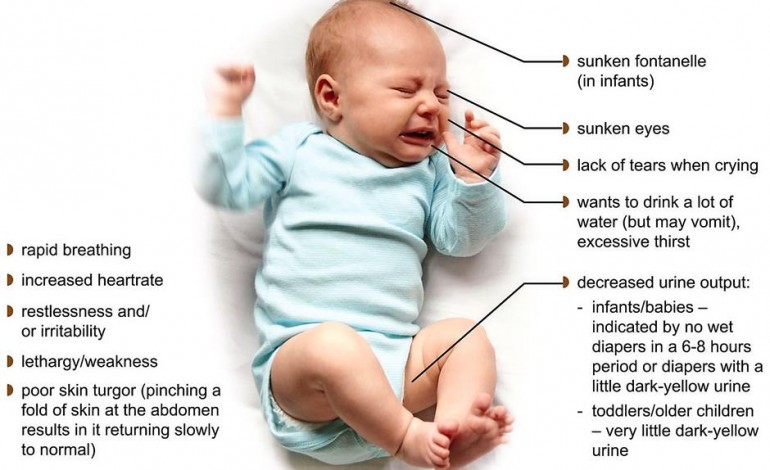
Infants are particularly susceptible to the ill effects of dehydration because of their greater baseline fluid requirements (due to a higher metabolic rate), higher evaporative losses (due to a higher ratio of surface area to volume), and inability to communicate thirst or seek fluid. Infants and toddlers remain some of the most vulnerable groups, especially for dehydration, along with elderly persons who lack a sense of thirst as they age. It is the designer’s job to protect and care for the vulnerable.
It can be so easy for parents to forget to provide their young child with adequate hydration, especially when they’re sick. Most do not know the ideal water regimen which can range from 4 oz. to 8 cups a day and can greatly vary depending on health, body weight, and water output. Not to mention, that they have 100 things running through their head to take care of their child’s health, including tracking medication intake, temperature, and many other concerning symptoms that can arise at any point. This influx of things to remember and treatments to administer causes parents additional stress and most report feelings of anxiety and being overwhelmed while their child is sick.
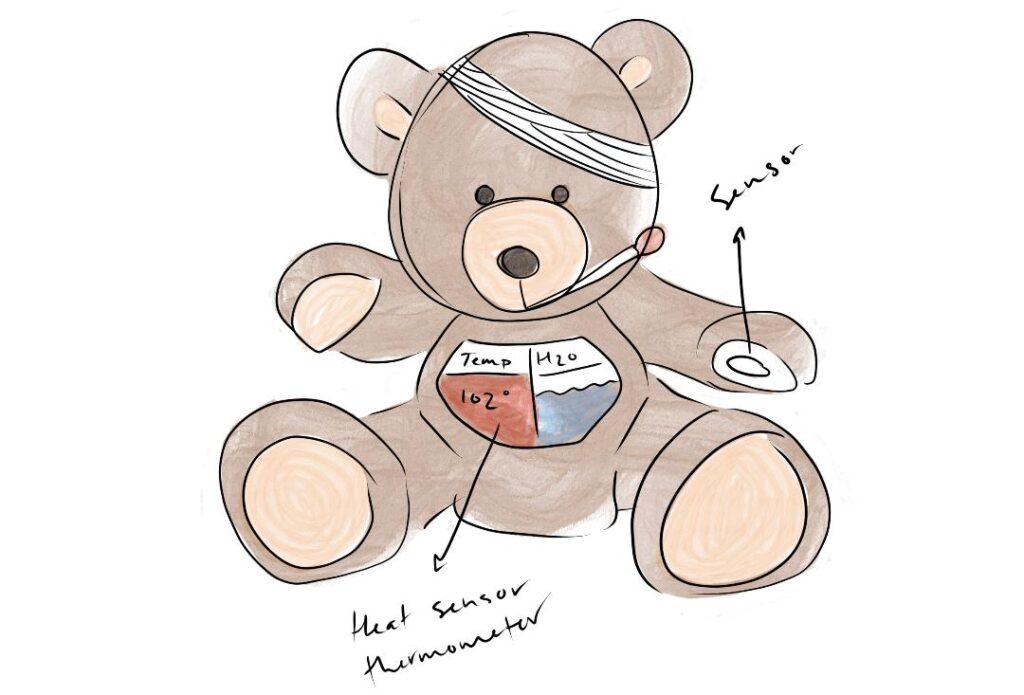
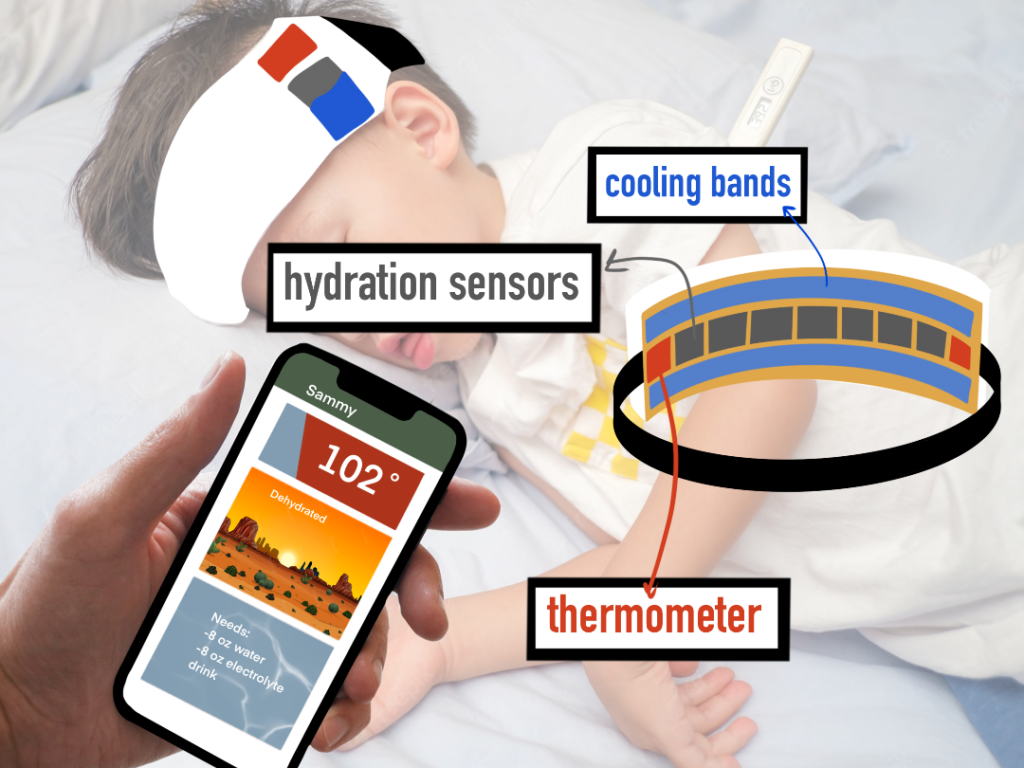
In an attempt to treat and bring awareness to dehydration, Priority Designs is working with OSU Industrial Design students to design wearable technology products to monitor dehydration. The objective is to create a wearable product that tracks health symptoms, including but not limited to hydration levels and alerts the caretakers of levels and treatment tips.

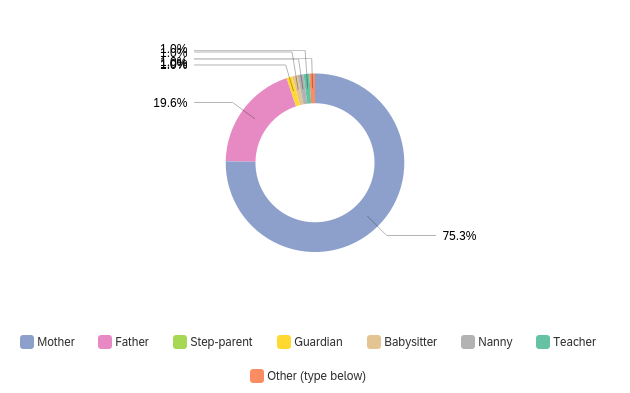
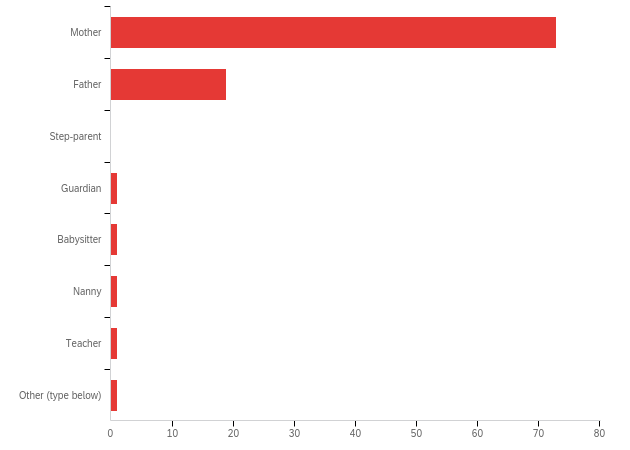
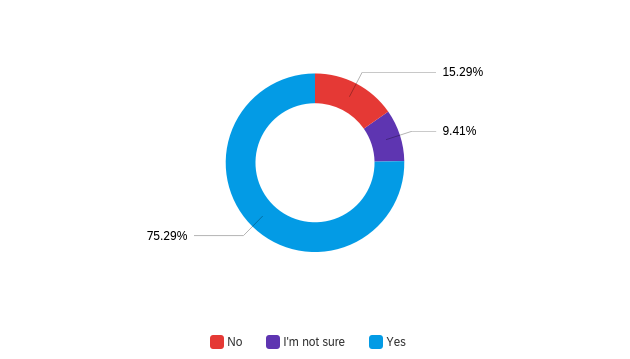
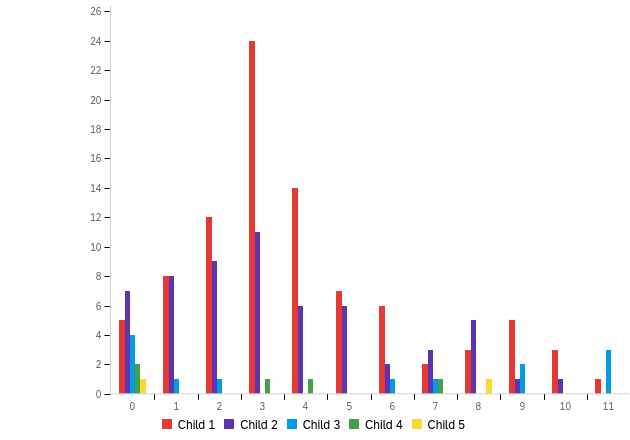
Secondary research was conducted in the topics of Science and Technology, Business, Focus, and Arts to gain an understanding of the published findings surrounding the topic and identifiable problem. Surveys were then sent out to parents, teachers, nannies and other caretakers of young children who have had first hand experience caring for sick children. 99 responses were recorded reporting a number of important findings regarding high levels of stress surrounding care and trends in actions by caretakers. It was found that over 98% of caretakers feel negative feelings while caring for their sick child including stress, anxiety, sadness and feeling overwhelmed. 29% of parents report they cannot tell when their child is dehydrated and 25% report they do not take measures to monitor their child’s hydration while they are sick. Of the 71% who believe they can tell when their child is dehydrated, when prompted in follow up interviews, reported they use methods such as diaper counting, dry mouth observations, and monitoring urine color. These same parents responded that they were not always sure of the accuracy of these methods and “did their best”. Of the 6 parents interviewed, 3 mentioned unprompted that they were more anxious about dehydration when their child was an infant given that infants are more immuno-compromised and there are so many health issues made aware to them by doctors and media. While low diaper count, dark urine color, and observations of dry mouth are some indicators of dehydration, they are some of the last signs that show that the child has been dehydrated for much too long at that point.
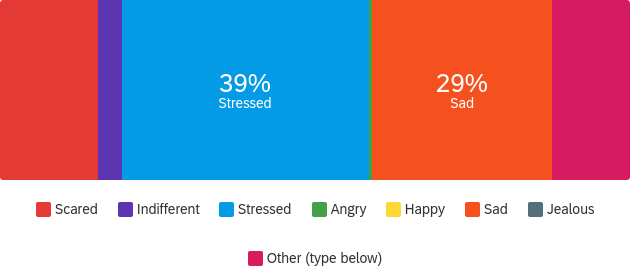
All parents interviewed had some experience with smart technology, and 5 out of the 6 utilized a smart health tracking app when their child was an infant. They found it helpful to have another source to remind them what to look out for. 5 out of the 6 said they would find it useful to have access to their child’s data. One parent expressed her belief that access to such data would in fact greatly increase her already high anxiety surrounding her child’s health. For this reason, any complementary app design needs to be designed very intentionally so as to not add additional mental health problems to the caretaker while still focusing on the main intention to help alleviate physical health concerns of the child.
Following the one-on-one interviews, I was able to set up a workshop at Balanced Family Academy in Clintonville, Ohio. During this workshop I plan to utilize Co-Design activities to further product development and understanding of user needs. I will do so by prompting participants to sketch design concepts of their own and review a collection of my own. This is not for review on feasible products but as an attempt to gain perspective on a number of possible design components, split among multiple underachieving products. By receiving feedback on what users do NOT like about each product, I will gain a better understanding of what they do want, something users do not always have the ability to know or communicate.


Given that infants and toddlers are incapable of taking care of or communicating their own needs, it was vital to do a lot of research through the vantage point of the caretaker as the stakeholder. While the wearable design aims to physically care for the infant, to monitor their dehydration, it also aims to care for the mental health of the caretaker, in a lot of cases the parent. By providing a tool for the parent to care for their infant or toddler, it alleviates stress that allows them to provide more care in other areas. This alleviation will not only be focused on hydration tracking. It is apparent that parents are monitoring much more than hydration and are unlikely to search out or utilize a product that only tracks hydration. The goal of this design is to alleviate pressure on caretakers through the tracking of multiple health factors including temperature, medication intake, and any other unexpected symptoms that may arise.
Sources:
Canavan, A., & Billy S. Arant, J. (2009, October 1). Diagnosis and management of dehydration in children. American Family Physician. Retrieved September 5, 2022, from https://www.aafp.org/pubs/afp/issues/2009/1001/p692.html
Mayo Foundation for Medical Education and Research. (2021, October 14). Dehydration. Mayo Clinic. Retrieved August 25, 2022, from https://www.mayoclinic.org/diseases-conditions/dehydration/symptoms-causes/syc-20354086
Cafasso, J. (2016, June 2). Signs of dehydration in toddlers: Warning signs. Healthline. Retrieved August 25, 2022, from https://www.healthline.com/health/parenting/signs-of-dehydration-in-toddlers#when-to-see-a-doctor




