Author: Mayo Clinic
Published Aug. 30, 2024
“Mayo Clinic has extensive experience with the use of sEEG to localize seizure onset sites in children. “High-quality brain imaging is critical prior to sEEG to guide electrode implantation,” says Mayo Clinic neuroradiologist Brian J. Burkett, M.D., M.P.H.
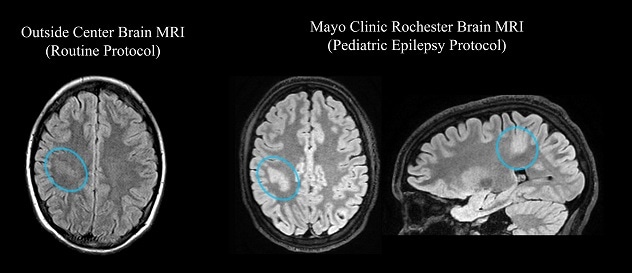
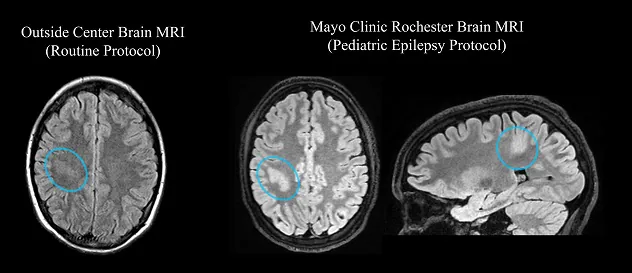
Optimized epilepsy protocol
MRIs from a 14-year-old patient with epilepsy. Left. A lesion (blue circle) is difficult to see on an image obtained elsewhere. Right. The lesion (blue circles) stands out clearly on MRI performed with Mayo Clinic’s optimized MRI protocol. The dedicated epilepsy protocol includes 3D image acquisition, enabling confirmation of the lesion in multiple spatial planes.
Mayo Clinic specialists use an MRI protocol specific to pediatric epilepsy. The protocol is optimized to show various types of abnormalities that might cause seizures.
“In many cases, these abnormalities are subtle and could be obscured or even invisible on an MRI of lower quality,” Dr. Burkett says. “Review by experienced neuroradiologists also maximizes the chance of detecting abnormalities. Prior to sEEG, cases are reviewed by several Mayo Clinic neuroradiologists with expertise in epilepsy imaging.”
Additional brain imaging techniques that might be used include:
- Skull base CT.
- Subtracted ictal and inter-ictal SPECT (SISCOM) and statistically normalized subtraction coregistered to MRI (STATISCOM).
- Positron emission tomography (PET)-CT.
- PET-MRI.
Localizing seizure onset sites with sEEG means children avoid craniotomy and generally have shorter hospital stays. “Once the electrodes are removed, patients often leave the hospital the next day,” Dr. Wong-Kisiel says.
sEEG also allows more time to consider treatment options. “Since there’s no craniotomy, the decision about therapy doesn’t need to be made right away,” Dr. Wong-Kisiel says. “Surgery is a big step. sEEG allows parents more time to be comfortable with making decisions.”
The procedure might be combined with ablation. “There is an option to add radiofrequency ablation to the electrodes that are recording during sEEG in areas identified as seizure focus sites,” Dr. Wong-Kisiel says. “About 40% of patients might have some benefit in terms of seizure reduction.”
Minimally invasive treatments
Once neurodiagnostic monitoring is completed, Mayo Clinic’s pediatric epilepsy team meets to determine optimal treatment. LITT may be used to ablate focal epileptogenic regions previously treated with an open craniotomy approach.
Corpus callosotomy might be considered for children experiencing generalized onset atonic or tonic seizures. The procedure eliminates or markedly decreases these drop seizures for most children. Mayo Clinic subspecialists have experience using LITT to perform corpus callosotomy. “Laser callosotomy is significantly less invasive than open callosotomy, which involves craniotomy, dissection and brain retraction,” says Mayo Clinic pediatric neurosurgeon Kai J. Miller, M.D., Ph.D.
Neurostimulation therapies, which aren’t commonly used to treat pediatric epilepsy, also are an option for focal and generalized epilepsy. Stimulation might be trialed in areas indicated by sEEG during that procedure. Mayo Clinic offers responsive neurostimulation, deep brain stimulation, vagus nerve stimulation and subthreshold cortical stimulation.” (Mayo Clinic, 2024)
One factor for my capstone that I had not quite explored or thought about too much was my demographics. Who do I want my product to be designed. Considering demographics in my process can have effects on the final design. Should it be accommodating to all or should there be a specialized group that it is intended. This article brings to attention the relationship of children and epilepsy. These individuals are so young and experiencing a harsh condition. The choices that their parents, their doctors, their nurses and ultimately the designers of their medical products can affect them for the rest of their whole life. Being conscious of the responsibility that we have as designers really comes into light when we think about our designs having life lasting effects. If a component is overlooked in a medical device, and an incident occurs, that child could be permanently physically or emotional disabled for the remainder of their life.
When designing for children it is also useful to take into account the physiological differences. The ergonomics, the complexity, the duration of use could all be different. Children have different mental understandings of medical topics and medical intervention. How, through my designs, can I accommodate these children’s fears and comfort level. Children are often assisted when in healthcare because they are still minors. Thinking about the caretakers role in their medical assistance can be impactful when designing. This article was insightful for my capstone project and raised questions that I now can further explore.
Reference
Kaye Clinic. Mayo Foundation for Medical Education and Research. (2024, August 30). Innovative strategies for pediatric epilepsy. Mayo Clinic. https://www.mayoclinic.org/medical-professionals/neurology-neurosurgery/news/innovative-strategies-for-pediatric-epilepsy/mac-20571956