Patients’ perceived burdens of their health problems play an important role in the consultation. Information gathering of these perceptions is considered as part of the “groundwork for explanation and treatment planning”.1 Older patients, however, often do not present with just one but multiple morbidities. Rather than deciding upon treatment for a single condition, doctors need to factor multiple health problems into one holistic treatment plan.2 In these circumstances, patients’ views on their disease-specific burdens need to be simultaneously collected and weighed in relation to one another.3,4 In practice, however, physicians gather views on single diseases in a subsequent way,5 and there is no clear strategy on how to strike a balance between different health-related burdens.
The phrase “burden” is introduced in this context to depict illness perceptions associated with negative impacts of a health problem. The underlying concept of illness perceptions used here is Leventhal’s common-sense model of illness representation. In this model, the individual is seen as a problem solver, who evaluates a health problem on the cognitive and emotional level. The cognitive themes center around the disease label, its perceived timeframe, causal attributes, controllability, and consequences. In parallel, emotional responses gain momentum with feelings such as depression, annoyance, anger, or anxiety.6 Hence, the perceived burden of a health problem is influenced by personal emotional and cognitive appraisals, both of which need to be represented in an assessment of burden.
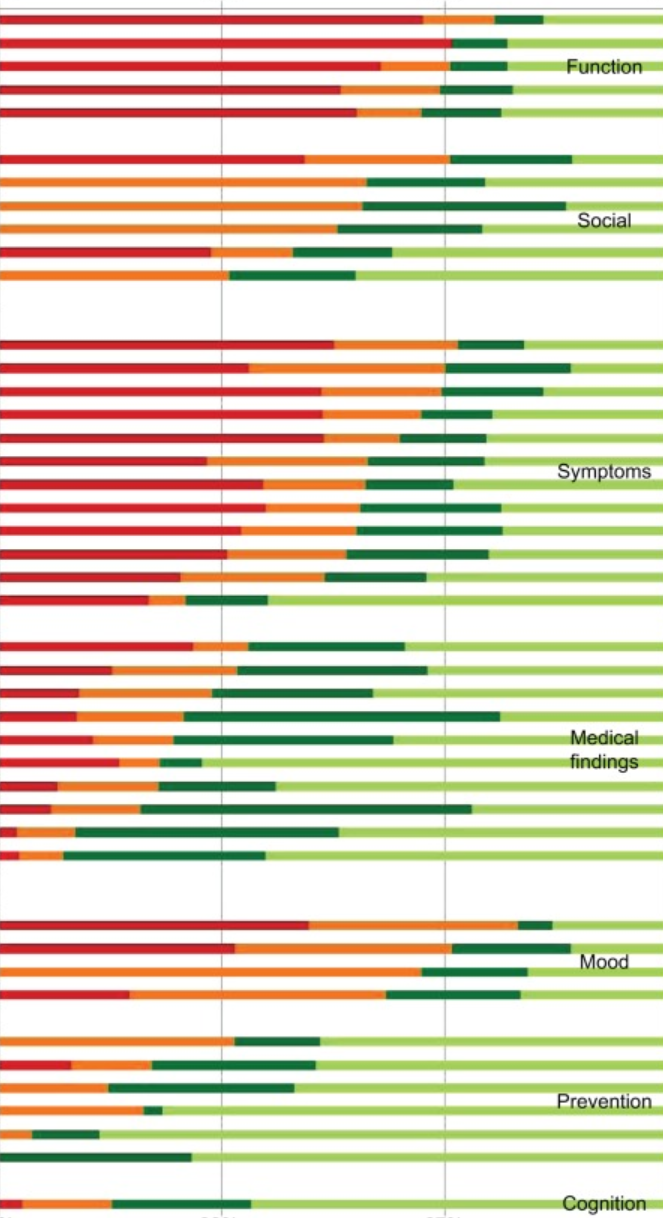
Perceived burden is usually assessed using two common approaches: generic measures across diseases or measures for specific conditions. An example of a generic measure is self-rated health. Population studies demonstrate a general decrease in self-rated health with advanced age and the presence of diseases.7 Other instruments measure burden for a specific condition or context, such as claudication or the caregiver’s burden.8,9 Both approaches cannot be applied to assess burdens of multiple health problems within a person, and instruments that measure or rank multiple burdens are not yet established. A good platform to develop such an assessment of multiple burdens seems to be the Duke/WONCA Severity of Illness Checklist. The original version assesses the severity of health problems for a patient from a professional point of view. A modified version was developed later to capture the patient’s perspectives on his or her health problems.10 We chose this patient version to measure perceived burden, and pilot tested and revised it in an earlier study.11
The negative impact of multiple morbidities on health-related quality of life has implications for clinical practice.12 Care decisions cannot be solely justified by guidelines for single diseases. Rather, patient-related burdens and treatment preferences need to be factored into the complex decision-making process.13 However, there appears to be a research gap in surveying and understanding the differential burden for patients with multimorbidity. The current study aims to examine perceived burdens of older patients of their different health problems.
Overview:
Researchers need to take a closer look at how patients, in this case elder patients with multiple long-term health problems, perceive their own health issues. A patient’s emotional and mental perception of their wellbeing is often overlooked as inferior in importance to their physical symptoms. This study looks at the perceived “burden” that elderly patients feel due to their overall health. It implies that the patient’s preferences and mental perspectives regarding their care should be taken into account, while also including the entirety of their ailments (not necessarily treating ailments individually).